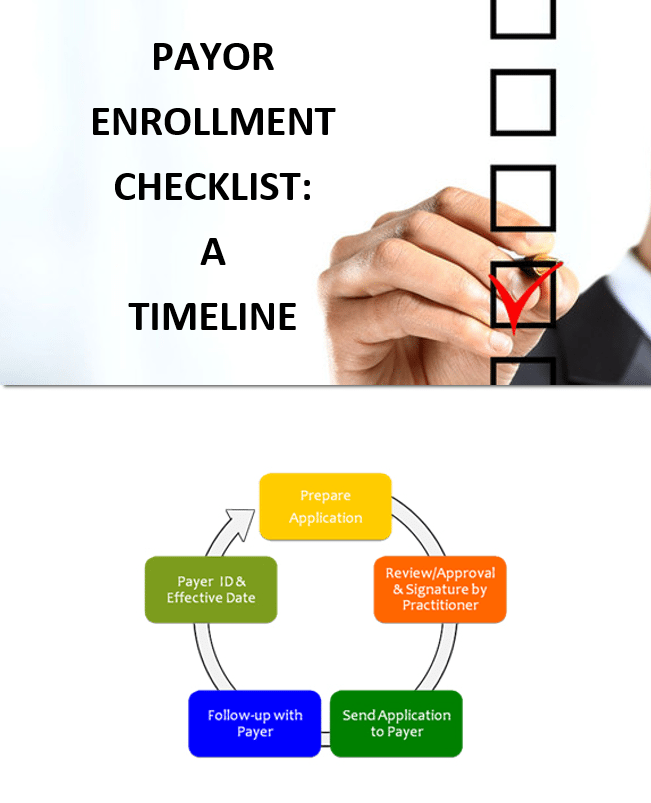
This whitepaper contains information on each step of the payor enrollment process, including how long it should take for each step to be completed.
You will learn about the following steps in the enrollment process:
- Start the process early!
- Review approval and signature by practitioner 60-90 days out.
- Follow-up with payor 30 days out.
… and more!





